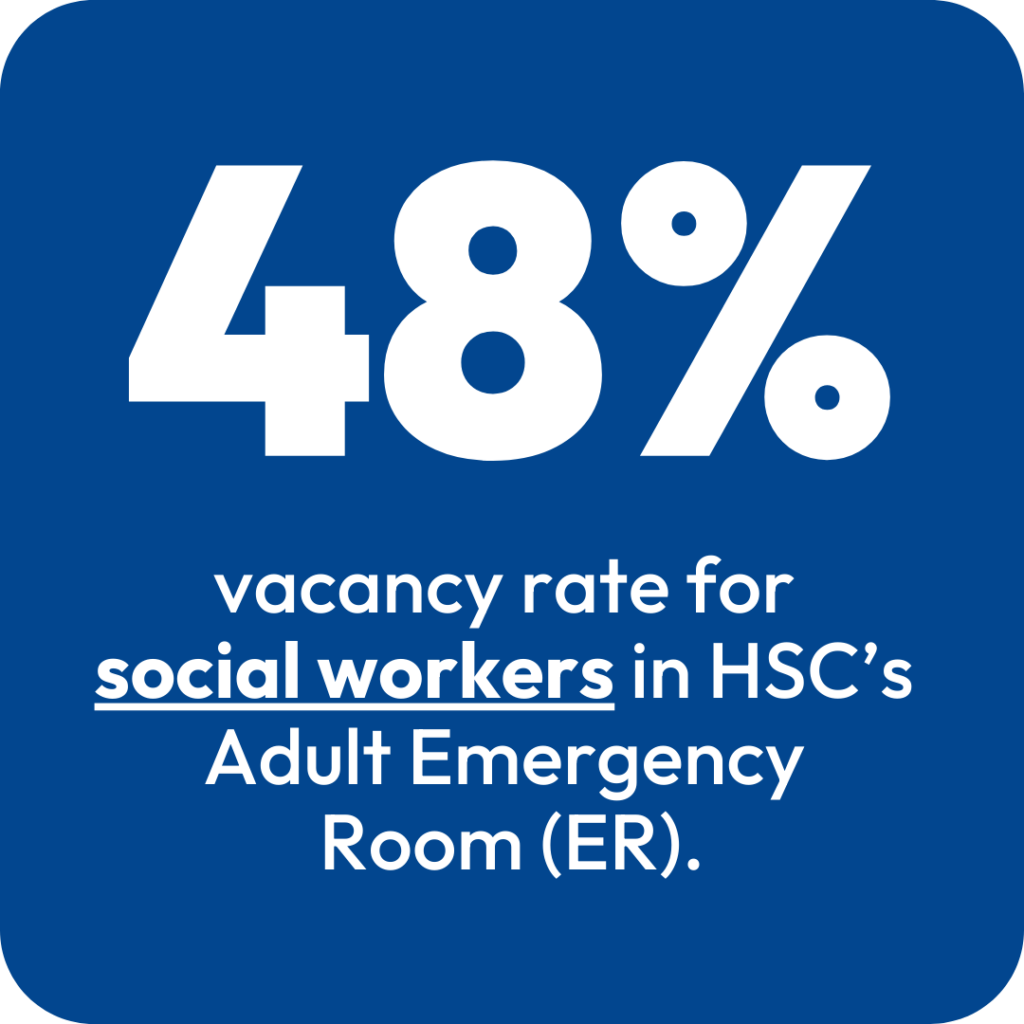
Social workers are vital to getting patients discharged safely, freeing up beds and reducing emergency room (ER) wait times. As the vacancy rate for social workers in HSC’s ER rises to 48%, wait times are also increasing.
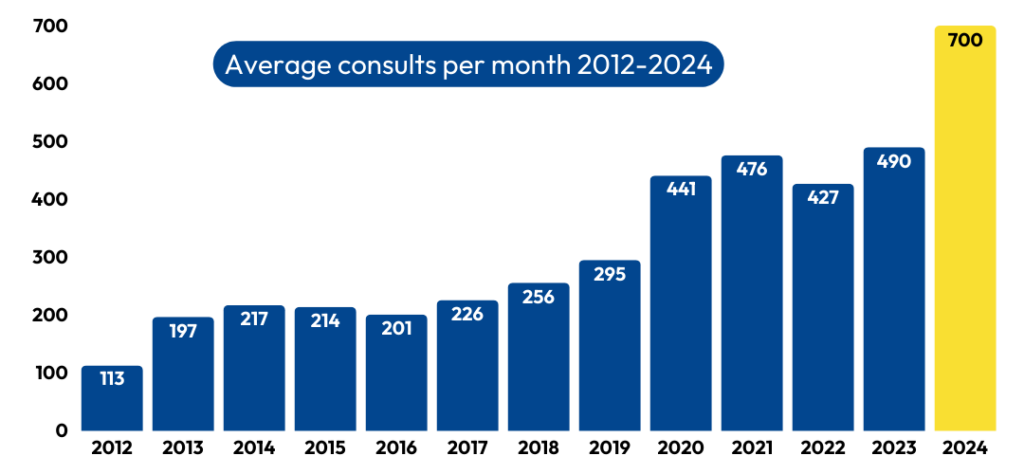
In the ER, social workers provide critical services to patients with increasingly complex needs, and the reality is, caseloads for HSC’s ER social workers have increased dramatically in 2024 compared to previous years.
As skilled problem-solvers, social workers find creative solutions to meet the full needs of each patient. This may look like accessing affordable medications, connecting patients with substance-abuse resources, assisting with housing, or speeding up discharge plans.
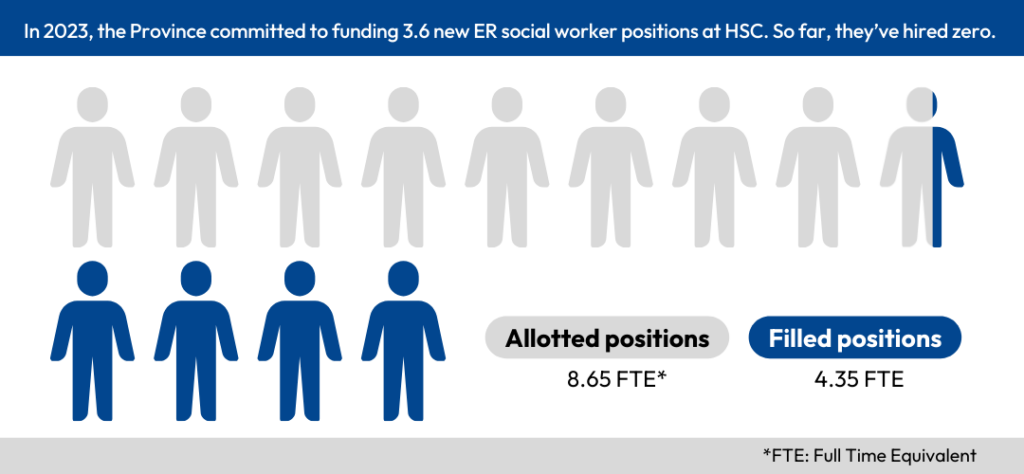
During the Throne Speech on November 7, the Province announced continued support for a commitment they made last fall: hiring more allied health professionals, such as social workers, to discharge patients with complex needs seven days a week. The original commitment included funding for 3.6 new social worker positions. So far, they’ve hired zero.
In fact, we have fewer social workers in HSC’s ER today than we did last year.
Social workers are consistently asked to do more with less, which impacts quality of care and puts the safety of patients and staff at risk.
Usually we say we can’t afford to go backwards. In this case, we HAVE gone backwards. Health-care leaders should be doing everything they can to support and retain these specialized allied health professionals.
“Enough is enough. Social workers in the ER have a profound impact on the patients they work with, and they are vital to solving ER wait times.
Jason Linklater
The current staff retention issues are unacceptable.”
MAHCP President