Manitoba’s rural communities deserve responsive, safe emergency medical services.
This week, the Province announced financial support for students and in-community training programs to recruit Emergency Medical Responders (EMRs) in rural Manitoba. While the announcement was framed as a way to increase ambulance coverage and shorten wait times, MAHCP is concerned about the level of care EMRs can provide in a critical emergency, which Health Minister Uzoma Asagwara called an “alternative level of care”. Manitobans aren’t looking for an alternative; they want the 200 paramedics the NDP government promised, only 18 of which have been added since October 2023.
“The bottom line is you need two fully trained paramedics to handle most emergency calls, including cardiac arrests, severe trauma, and unstable patients.”
JASON LINKLATER
MAHCP President
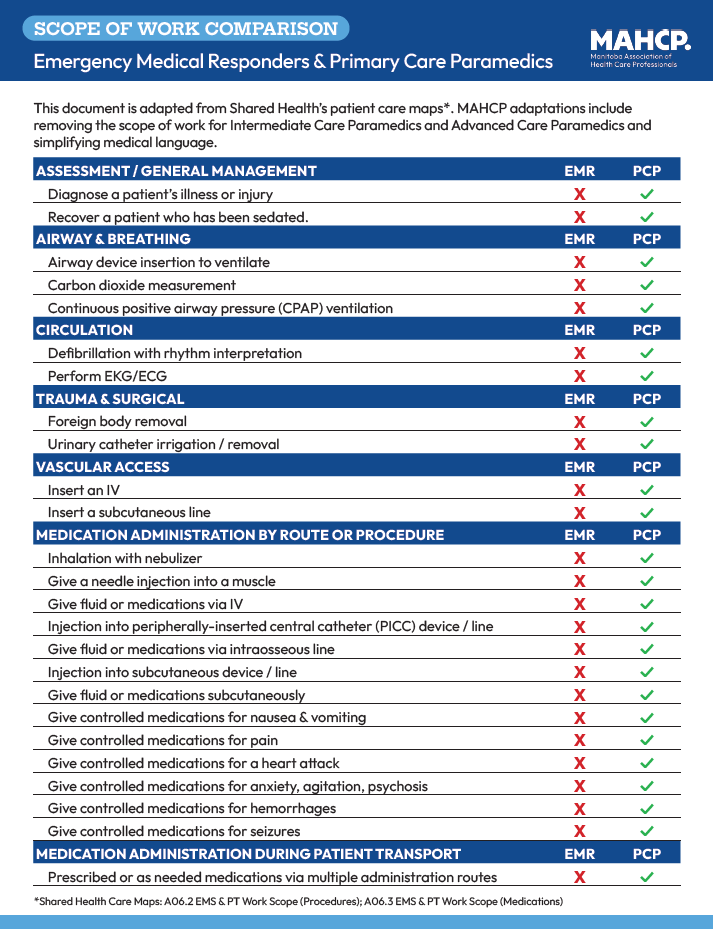
EMRs are valuable professionals who play an important role in supporting emergency medical services (EMS), particularly in stable patient transport and medical first response. However, their limited scope of practice and clinical training does not allow them to provide anywhere near the same level of care that paramedics can. Putting EMRs on ambulances rather than paramedics puts them, and patients, at risk.
“Shared Health and our provincial leaders are opting for fast and cheap — a long-term solution that isn’t good for rural Manitobans, or any Manitobans, when what you need is a highly skilled Primary Care Paramedic (PCP) to treat and stabilize a patient,” MAHCP President Jason Linklater said.
High-acuity, time-sensitive calls, such as cardiac arrests, severe trauma, violent or unstable patients, obstetrical crises, and complex medical emergencies, require simultaneous interventions from two fully-trained PCPs.
An EMR simply cannot replicate that level of care.
Shared Health is creating a dangerous situation for patients and staff, and putting more pressure on paramedics who are already burnt out from years of short-staffing and excessive overtime.
Let’s be clear: MAHCP is not advocating against EMRs. They play an important role in EMS. We’re advocating for solutions designed to protect patients, reduce paramedic burnout, and support a fully-trained paramedic workforce that can deliver emergency care at the highest standard — the standard the province once committed to. So far, Shared Health and the Province have not implemented any of the common-sense and cost-effective solutions MAHCP has put forward.
“Something has to be done, but let’s do it the right way to ensure we are solving a long-term problem, and not just a Band-Aid that becomes a permanent Band-Aid in the future.”
If the government is serious about improving rural EMS, it needs to:
- Improve Shared Health hiring practices to ensure continuous hiring and onboarding of PCPs, including posting and filling all vacancies promptly, and providing incentives for hard-to-fill positions.
- Expand the number of PCP training seats, and include options for distance or distributed learning models to make PCP training more accessible for rural Manitobans.
- Cover tuition for PCP training, including, but not limited to, EMR-path students.
- Require new EMRs to complete PCP training within a defined period of time, and provide paid time off and financial support for that training, to ensure the EMR path truly becomes a bridge to the professional paramedic workforce Manitobans were promised.
- Cover costs of travel, accommodation, and further monetary incentives for rural paramedics to fill gaps in hard-to-fill areas.